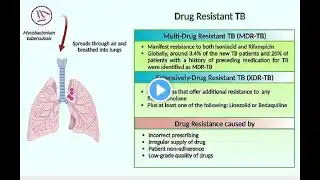
Typical Treatment Regimens for Multi Drug Resistant Tuberculosis
Typical treatment regimens for multidrug-resistant tuberculosis (MDR-TB) involve combinations of second-line drugs such as bedaquiline, linezolid, fluoroquinolones, and clofazimine, often given for 9–20 months depending on the patient’s condition and drug resistance profile. These regimens are more complex, costly, and associated with higher risks of side effects compared to standard TB treatment. 🔑 Key Points on MDR-TB Treatment Definition: MDR-TB is resistant to at least rifampicin and isoniazid, the two most powerful first-line TB drugs. Core Drugs Used: Bedaquiline – cornerstone of modern MDR-TB regimens. Linezolid – highly effective but can cause bone marrow suppression and neuropathy. Fluoroquinolones (levofloxacin, moxifloxacin) – critical for backbone therapy. Clofazimine – often included for its bactericidal activity. Cycloserine, delamanid, or ethionamide – used depending on resistance profile. Treatment Duration: Typically 9–20 months, shorter regimens are possible if resistance is limited and patient response is good. Individualization: Regimens are tailored based on drug susceptibility testing, patient tolerance, and comorbidities. 📋 WHO-Recommended MDR-TB Regimens Regimen Type Duration Key Drugs Notes Short regimen 9–11 months Bedaquiline, fluoroquinolone, clofazimine, pyrazinamide, ethambutol, high-dose isoniazid Used when resistance is limited; faster completion. Long regimen 18–20 months Bedaquiline, linezolid, fluoroquinolone, clofazimine, cycloserine Standard for most MDR-TB cases; higher toxicity risk. Individualized regimen Variable Based on drug susceptibility testing Necessary for pre-XDR or XDR-TB (extensively resistant TB). Sources: ⚠️ Challenges Side effects: Neuropathy, QT prolongation, gastrointestinal issues. Cost: MDR-TB regimens cost 4–12 times more than drug-susceptible TB treatment. Adherence: Long duration and toxicity make adherence difficult, requiring strong patient support systems. #Tuberculosis