Full Vignette with Extended Explanations, Neuronal Physiology, Physiology, USMLE Step 1
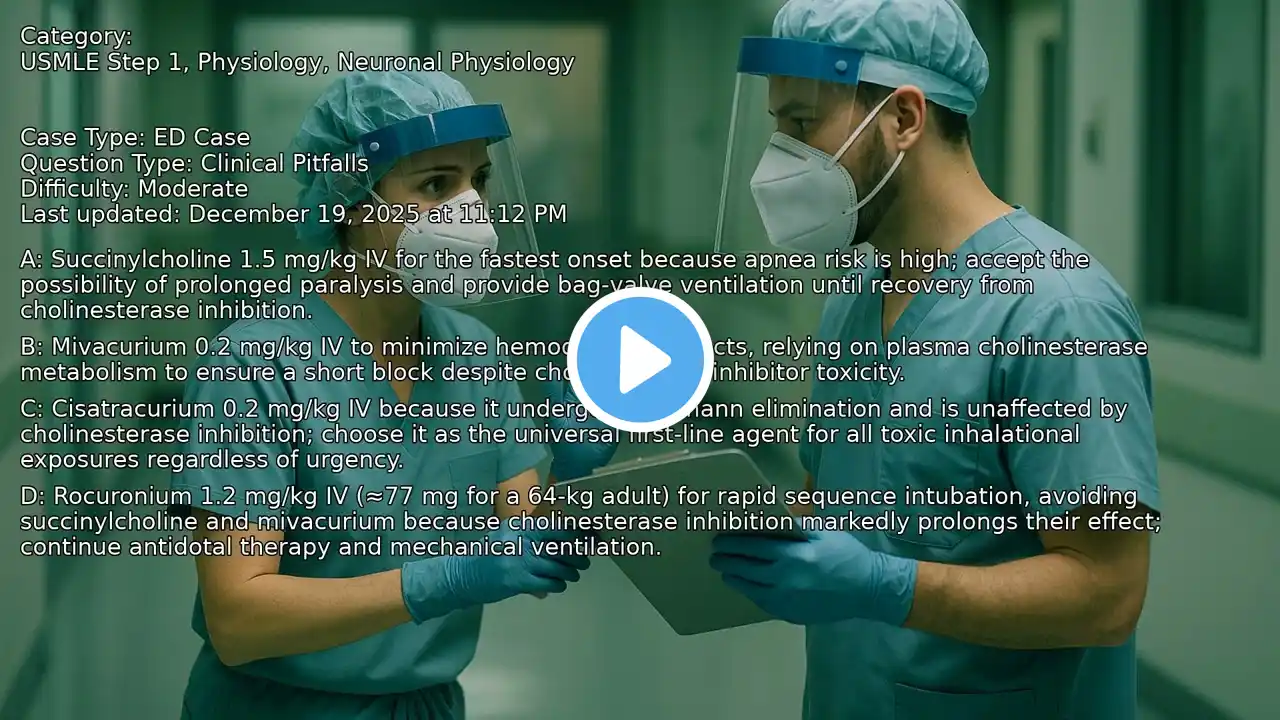
Understanding organophosphate poisoning and its complications is crucial for emergency medicine practitioners, especially in rural or resource-limited settings. This video breaks down a real-world case of delayed neuromuscular respiratory failure-known as 'intermediate syndrome'-that can occur 24-96 hours post-exposure, even after muscarinic symptoms are controlled. Master the pathophysiology and essential management strategies to effectively support patients during extended transfer delays. VIDEO INFO Category: Neuronal Physiology, Physiology, USMLE Step 1 Difficulty: Moderate - Intermediate level - Requires solid foundational knowledge Question Type: Natural History Case Type: Resource Limited QUESTION A 43-year-old manufacturing worker is brought to a small critical access hospital during an ice storm that has closed highways and grounded air transport; transfer is delayed an estimated 12-18 hours. He mixed agricultural pesticides earlier the same day.... OPTIONS A. A delayed neuromuscular junction failure ( intermediate syndrome ) 24-96 hours post-exposure with dominant nicotinic endplate dysfunction causing proximal limb and respiratory muscle weakness despite controlled muscarinic signs; prioritize ventilatory support and continue oxime therapy. B. A recurrent muscarinic cholinergic crisis from inadequate atropinization; repeat large atropine boluses now until bronchorrhea and wheeze fully resolve again. C. Organophosphate-induced delayed neuropathy that typically appears within 24-96 hours with distal sensory loss and foot drop, so ventilatory compromise is unlikely. D. Central hypoventilation from toxin-induced cortical hyperexcitability causing recurrent seizures; escalate benzodiazepines rather than respiratory support. CORRECT ANSWER A. A delayed neuromuscular junction failure ( intermediate syndrome ) 24-96 hours post-exposure with dominant nicotinic endplate dysfunction causing proximal limb and respiratory muscle weakness despite controlled muscarinic signs; prioritize ventilatory support and continue oxime therapy. EXPLANATION After apparent stabilization of muscarinic symptoms with atropine and oxime therapy, this patient develops progressive neck flexor and proximal limb weakness with shallow respirations and rising end-tidal CO2 about 36 hours after presumed organophosphate exposure. Clear mentation, absence of recurrent bronchorrhea or miosis, and a trend toward hypercapnic hypoventilation point away from a recurrent muscarinic crisis and toward a nicotinic problem at the neuromuscular junction. This time course and pattern are classic for the intermediate syndrome (IMS): delayed neuromuscular junction failure that typically emerges 24-96 hours after exposure, with involvement of proximal muscles and respiratory pump, often necessitating ventilatory support. The immediate priorities in a resource-limited ED are airway/ventilatory support (including noninvasive ventilation if feasible while arranging transfer) and continuation of oxime therapy, recognizing ongoing debate about oxime efficacy but the practice standard to continue when available. The alternatives misinterpret timing and physiology.... --------------------------------------------------- Our cases and questions come from the www.EndlessMedical.Academy quiz engine - multi-model platform. Each question and explanation is forged by consensus between multiple top AI models (GPT, Claude, Grok, etc.), with automated web searches for the latest research and verified references. Calculations (e.g. eGFR, dosages) are checked via code execution to eliminate errors, and all references are reviewed by several AIs to minimize hallucinations. Important note: This material is entirely AI-generated and has not been verified by human experts; despite stringent consensus checks, perfect accuracy cannot be guaranteed. Exercise caution - always corroborate the content with trusted references or qualified professionals, and never apply information from this book to patient care or clinical decisions without independent verification. Clinicians already rely on AI and online tools - myself included - so treat this book as an additional focused aid, not a replacement for proper medical education. Visit www.endlessmedical.academy for more AI-supported resources and cases. This material can not be treated as medical advice. May contain errors. ---------------------------------------------------