12. Guidelines For Multi- Drug Resistant TB & Extensively- Drug Resistant TB: Pharmacology Lectures
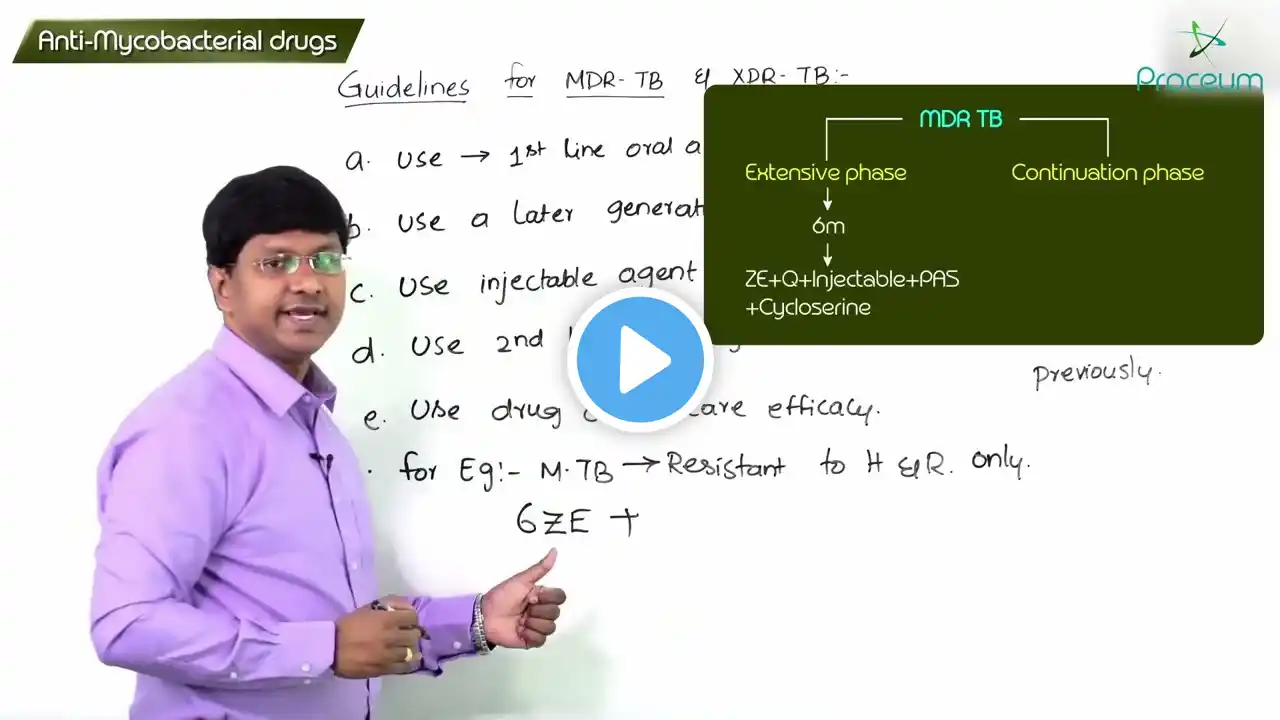
𝐒𝐮𝐛𝐬𝐜𝐫𝐢𝐛𝐞 𝗙𝐨𝐫 𝗠𝐨𝐫𝐞 𝗜𝐧𝐟𝐨𝐫𝐦𝐚𝐭𝐢𝐨𝐧 𝐨𝐧 𝗛𝐞𝐚𝐥𝐭𝐡 👩⚕ 𝐚𝐧𝐝 𝗠𝐞𝐝𝐢𝐜𝐢𝐧𝐞💉🩺💊 📌𝗜𝗻𝘀𝘁𝗮𝗴𝗿𝗮𝗺 : / clinical.learning 12. Guidelines For Multi- Drug Resistant TB & Extensively- Drug Resistant TB: Pharmacology Lectures ----------------------------------------------------------------------------------------------------------------------- MDR-TB (Multi-Drug Resistant Tuberculosis) and XDR-TB (Extensively Drug-Resistant Tuberculosis) are severe forms of drug-resistant TB caused by Mycobacterium tuberculosis strains that do not respond to conventional first-line anti-TB drugs 💊🦠. MDR-TB is resistant to Rifampin (RIF) and Isoniazid (INH), while XDR-TB is resistant to Rifampin, Isoniazid, Fluoroquinolones (e.g., Levofloxacin, Moxifloxacin), and at least one second-line injectable drug (e.g., Amikacin, Capreomycin, Kanamycin) 🚨🩸. These drug-resistant forms of TB require prolonged treatment (≥18-24 months), multiple drugs, and strict monitoring to prevent treatment failure, transmission, and mortality ⚠️🏥. 🔹 WHO Guidelines for MDR-TB & XDR-TB Treatment: Shorter MDR-TB Regimen (9-12 months): Used in eligible patients who have not been exposed to second-line drugs and do not have fluoroquinolone resistance 🔄💊. Longer MDR-TB Regimen (18-24 months): For patients with extensive disease, prior treatment failure, or fluoroquinolone resistance 📉🛑. All-oral drug regimens are preferred over injectable agents to improve compliance and reduce ototoxicity (hearing loss) from aminoglycosides 🎧🚫. 🔹 Recommended Drug Regimens for MDR-TB/XDR-TB: Group A (Most effective, must be included): Levofloxacin/Moxifloxacin (Fluoroquinolones), Bedaquiline (ATP Synthase Inhibitor), Linezolid (Protein Synthesis Inhibitor) 🏆🔬. Group B (Add if needed for regimen completion): Clofazimine, Cycloserine/Terizidone (Cell wall inhibitors, CNS penetration) 🧬🩺. Group C (Used when Group A & B drugs cannot be used): Ethambutol, Delamanid, Pyrazinamide, Imipenem-Meropenem, Amikacin, PAS (Para-Aminosalicylic Acid) 💥🦠. 🔹 Newer Drugs in MDR/XDR-TB: Bedaquiline (FDA-approved): A diarylquinoline that inhibits mycobacterial ATP synthase, essential for energy production. It improves MDR-TB cure rates but has QT prolongation risk, requiring ECG monitoring 🫀📉. Delamanid: Inhibits mycolic acid synthesis, improving treatment success, but also prolongs the QT interval, requiring ECG monitoring 📊🩸. Pretomanid (used in BPaL regimen): A novel drug combined with Bedaquiline + Linezolid for highly resistant TB cases 🏆💡. 🔹 Challenges in MDR-TB & XDR-TB Treatment: Prolonged therapy (18-24 months), causing poor patient adherence and high treatment dropout rates ⚠️🩺. Severe side effects (Ototoxicity, nephrotoxicity, hepatotoxicity, myelosuppression, QT prolongation) requiring frequent monitoring 🎧💀. Expensive and limited access to second-line and novel TB drugs, especially in resource-limited settings 🌍💰. Drug interactions with ART (HIV-TB co-infection), requiring careful selection of compatible drugs 🦠💊. 🔹 Preventive Measures & Global Control Strategies: Rapid Drug Susceptibility Testing (DST) to identify drug resistance early and select appropriate treatment 📉🔬. Strict adherence to Directly Observed Therapy Short-Course (DOTS) programs to ensure patient compliance 📊🏥. BCG vaccination and early case detection to prevent transmission 🌍🛡️. Expanding access to novel MDR-TB/XDR-TB drugs (Bedaquiline, Delamanid, Pretomanid) and improving treatment protocols 💉💊. 🔹 Conclusion: MDR-TB & XDR-TB require aggressive treatment with second-line drugs, careful monitoring, and global TB control measures to prevent further resistance and improve patient survival 🌍💊. #MDRTB #XDRTB #TBResistance #WHOguidelines #Bedaquiline #Fluoroquinolones #TBPrevention #TBControl #LungHealth #TBHIV #DOTS #SaveLives #TBEradication #USMLE #NEETPG #GlobalHealth #StopTB #MycobacteriumTuberculosis #Pharmacology